- Giving
22 Jumps
22 Jumps aims to bring new hope to individuals and families affected by TBI and suicide. Due to a lack of objective diagnostic tools and effective treatment solutions, the “invisible
Brain trauma affects millions. Learn about traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD) and how they impact civilians and Veterans.

Understand brain trauma (TBI/PTSD) and the current state of research.
TBI symptoms, diagnosis, treatment, and the impact of our research.
PTSD symptoms, diagnosis, treatment, and the impact of our research.
Learn about suicide risk among military Veterans with brain trauma.
A new Community Coordination model to accelerate a first generation of diagnostics and treatments for Traumatic Brain Injury.
Cohen Veterans Bioscience is a non-profit 501(c)(3) biomedical research and technology organization dedicated to advancing brain health by fast-tracking precision diagnostics and tailored therapeutics.
Explore our Mission & Vision to advance solutions for brain trauma.
Meet the minds behind CVB.
Meet our Board of Directors.
A voice for the Veterans community.
Read stories from people living with brain trauma.
Interested in joining the team? Explore careers at CVB.
Connect with the experts at CVB.
Our approach is to build enabling platforms with strategic partners and to adopt a team science approach to fast-track solutions in years, not decades.

Fast-tracking diagnostics & therapeutics for brain trauma.
Advocating at the federal, state, and local levels.
Helping high-impact research succeed.
Driving quality & reproducibility in science.
Explore our research publications.
Advancing our understanding of invisible wounds.
Learn how to participate in clinical trials.
Fostering a collaborative approach to research.
Donate today to advance solutions for brain trauma. Together, we can advance research and improve lives.

Get the latest updates in PTSD & TBI research.
Share your story: how has TBI impacted you?
We look forward to hearing from you.
Learn about the latest news & events from CVB.
View press releases and more.
A new Community Coordination model to accelerate a first generation of diagnostics and treatments for Traumatic Brain Injury.
Established in 2017, the Coalition to Heal Invisible Wounds (Coalition), brings together leading non-profit organizations to advance a comprehensive research-focused advocacy agenda that addresses the invisible wounds of war and other significant comorbid conditions known to contribute to the suicide epidemic among Veterans and service members. The Coalition advocates for reforms to how the federal government prioritizes, manages, and funds brain health research, focusing on four key priorities: developing high-quality brain trauma therapies for Veterans and service members, adopting collaborative research roadmaps to guide the science, increasing the body of evidence on emerging therapeutic solutions, and ensuring full implementation of important mental health legislation. Learn more here.
The Navy SEAL Foundation (NSF) provides critical support for the warriors, veterans, and families of Naval Special Warfare (NSW) through a comprehensive set of over 30 programs under five Pillars of Support: Strength, Resilience, Health, Education, and Community. NSF is a high-performing organization committed to excellence. Charity Navigator has awarded it a 4-star rating since 2009 and a perfect score of “100” since 2014 for financial health, accountability, and transparency. The Foundation ranks higher than 99.9% of over 160,000 charities nationwide with ninety-three cents of every dollar donated directly funding its programs or being retained for future mission use. NSF is a 501(c)(3) national nonprofit charitable organization with TAX ID 31-1728910. It is not a part of the Department of Defense, or any of its components, and has no official affiliation with any federal entities. Learn more here.

The Green Beret Foundation (GBF) provides U.S Army Special Forces Soldiers and their families with emergency, immediate, and ongoing support. GBF assists over 5,000 Special Forces families each year. Since its inception, GBF has invested 84%, or 84 cents of every dollar, into its programs and services, which has totaled over $16 million that has directly supported the Regiment and its families. GBF is the only non-profit solely dedicated to supporting Green Berets and their families that has achieved a 4-Star Rating with Charity Navigator. Also, GBF is the sole Special Operations nonprofit organization that is accredited by the Department of Veterans Affairs for the purpose of preparation, presentation, and prosecution of disability claims. Get more information here.
TBI Fast Fact
19%
19% of Iraq and Afghanistan Veterans reported a probable TBI during deployment.
Veteran Suicide Fast Fact
14%
Veteran suicides make up a disproportionate 14% of total suicides in America.
Fast Fact
2.7 Million
TBI and PTSD have taken an enormous toll on Veteran populations with more than 2.7 million men and women deployed to support combat operations in Iraq and Afghanistan since 2001.
Fast Fact
Under 50%
Less than 50% of all veterans in need receive any type of mental health diagnosis or treatment.


Patrick Bellgowan, PhD, Deputy Associate Director, NINDS
Dr. Bellgowan shared an overview of TBI, including the causes of injury, categorized as blunt force, blast exposure, and penetrating injury. The factors impacting TBI are complex and interrelated, and include severity of injury, age, gender, injury type, history of prior TBI, genetics, and social determinants of health. Understanding the diagnostics and treatment of TBI is an evolving landscape. One of the issues facing experts is how to define and categorize TBI. The National Institutes of Health (NIH) are investing across the research spectrum with at least 11 of the institutes involved in the TBI portfolio. NINDS leads this work within NIH. Dr. Bellgowan shared that while federal agencies historically worked in silos on this issue, a 2012 Executive Order established the National Research Action Plan (NRAP), asking all federal agencies to work together to improve access to mental health services for veterans, service members, and military families. An interagency task force was established to implement the order and the Department of Health and Human Services (HHS), the Department of Veterans Affairs (VA), and the Department of Defense (DOD) have since coordinated efforts to combat TBI.
Dr. Ramoni followed and shared how the VA is contributing to the NRAP, first noting that to accelerate progress in TBI diagnosis and treatment we must build on the NRAP to more precisely diagnose sub-types of TBI that are similar in their types and length of symptoms and respond to the same treatments. An important path toward progress is to leverage data that already exists. The VA has data in their electronic health records dating back to 1999, which includes complete medical record information on 16.6 million veterans and partial information on another 10 million veterans. Additionally, the Million Veterans Program, a national research program to discover how genes, lifestyle, and military exposures affect health and illness, has data on over 830,000 veteran volunteers. The VA is working to establish a VA Data Commons in collaboration with the University of Chicago and the Open Commons Consortium. This will allow approved VA and non-VA researchers to access de-identified data from VA’s electronic health records. A pilot is expected to launch in 2022.
Rachel B. Ramoni, DMD, ScD, Chief Research & Development Officer, U.S. Department of Veterans Affairs

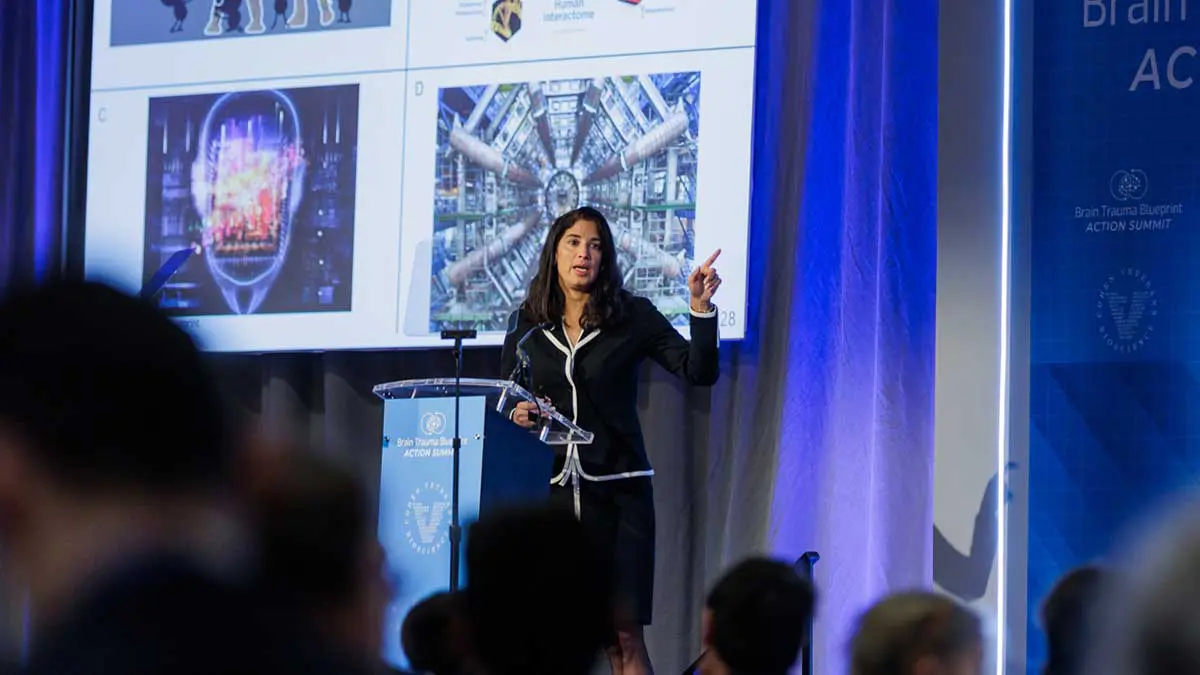
Magali Haas, MD, PhD, CEO & President, Cohen Veterans Bioscience
Next Dr. Haas discussed CVB’s mission to advance brain health by advancing precision medicine solutions. Dr. Haas shared an update on the Brain Trauma Blueprint, a roadmap to advance a first generation of targeted solutions for TBI, focusing on the chronic sequelae. The Brain Trauma Blueprint is born from the recognition that there are currently no FDA-approved therapies for TBI, and was the basis for the 2019 State of the Science Summit on TBI, which brought together over 100 thought leaders across the research ecosystem to identify the research gaps that have stymied progress as well as specific recommendations to overcome these gaps through a consensus research roadmap. The specific recommendations are to be published as part of a six part publication series in the Journal of Neurotrauma. If these efforts to align resources toward these gaps and priorities is successful, it will help catalyze a first generation of targeted treatments for TBI. The Brain Trauma Blueprint has already led to new public-private partnerships and collaborations, many of which were described in this briefing. Dr. Haas outlined some of the most pressing needs identified through the Brain Trauma Blueprint, including the need for a national surveillance system for all severities of TBI. At this time, the United States does not have a reliable method for tracking TBI; rather, it only tracks individuals affected by TBI based on emergency room encounters. It is important that a national surveillance system to track the number of individuals who sustain TBI, including those who do not seek care in an emergency setting.
Dr. Stone discussed his work toward developing a Normative Neuroimaging Library, supported by CVB. The field of neuroimaging is more than 100 years old. Since that time there has been significant expansion of capabilities around neuroimaging, but the ability to be able to pull information from the images and the clinical processes to interpret the images and manage care have remained relatively static. Current approaches are helpful for moderate to severe TBI where routine neuroimaging exams can reveal urgent findings. However, routine neuroimaging approaches have a relatively limited role in mild TBI and concussion, which constitute the vast majority of TBI seen in the U.S. In recent years, there have been advanced neuroimaging techniques that have allowed us to push the boundaries in what we can see, but these approaches require the acquisition of a large volume of images and require computational tools to derive certain measures. A Normative Neuroimaging Library will provide the foundational building blocks to bridge the gap between research and clinical applications for advanced neuroimaging and will address the rapidly expanding need for quantitative, diagnostic neuroimaging tools.

James R. Stone, MD, PhD, Associate Professor, Radiology & Medical Imaging, University of Virginia School of Medicine

Jamshid Ghajar, MD, PhD, President, Brain Trauma Foundation, Director, Stanford Brain Performance Center
The final speaker on the panel, Dr. Ghajar, discussed the Brain Trauma Blueprint and the impact of evidence-based solutions for diagnostics and treatment on coma, or severe TBI. Prior to the year 2000, there were no evidence-based guidelines in
place for individuals with severe TBI. Patients received very little brain pressure monitoring, were given steroids, were under-resuscitated and mortality was 50%. The Brain Trauma Foundation (BTF) created 21st century evidence-based guidelines calling for brain pressure monitoring, no steroids, no hyperventilation, full resuscitation and full feeding. As compliance with the guidelines went up, mortality went down, dropping to 25%. The CDC issued a report on the impact
of the BTF guidelines and similarly found a 50% decrease in death as well as
cost savings. Now the guidelines, which are constantly updated, are used in
every trauma center in the U.S. as well as internationally. The BTF continues to establish and update evidence-based guidelines for different areas including hospitals, ambulance care and the military. With the Brain Trauma Blueprint, there is a roadmap to move forward with further evidence-based solutions.
Dr. Matthew Rizzo, Chair of the American Brain Coalition, closed the briefing by encouraging Members of Congress to join the Congressional Neuroscience Caucus and Congressional Brain Injury Task Force and asked congressional staffers in the audience to support federal funding for biomedical research, including brain injury research.

The Brain Trauma Blueprint is a framework to advance precision diagnostics and therapeutics for brain trauma through a process of community stakeholder consensus roadmapping and collaborative execution. More information can be found here.
Cohen Veterans Bioscience is a non-profit 501(c)(3) biomedical research and technology organization dedicated to advancing brain health by fast-tracking precision diagnostics and tailored therapeutics.
Cohen Veterans Bioscience is a non-profit 501(c)(3) biomedical research and technology organization dedicated to advancing brain health by fast-tracking precision diagnostics and tailored therapeutics.
©2023 Cohen Veterans Bioscience | Privacy Policy | Terms of Use