First of six publications reports on new tool to identify patient subgroups that enable personalized care.
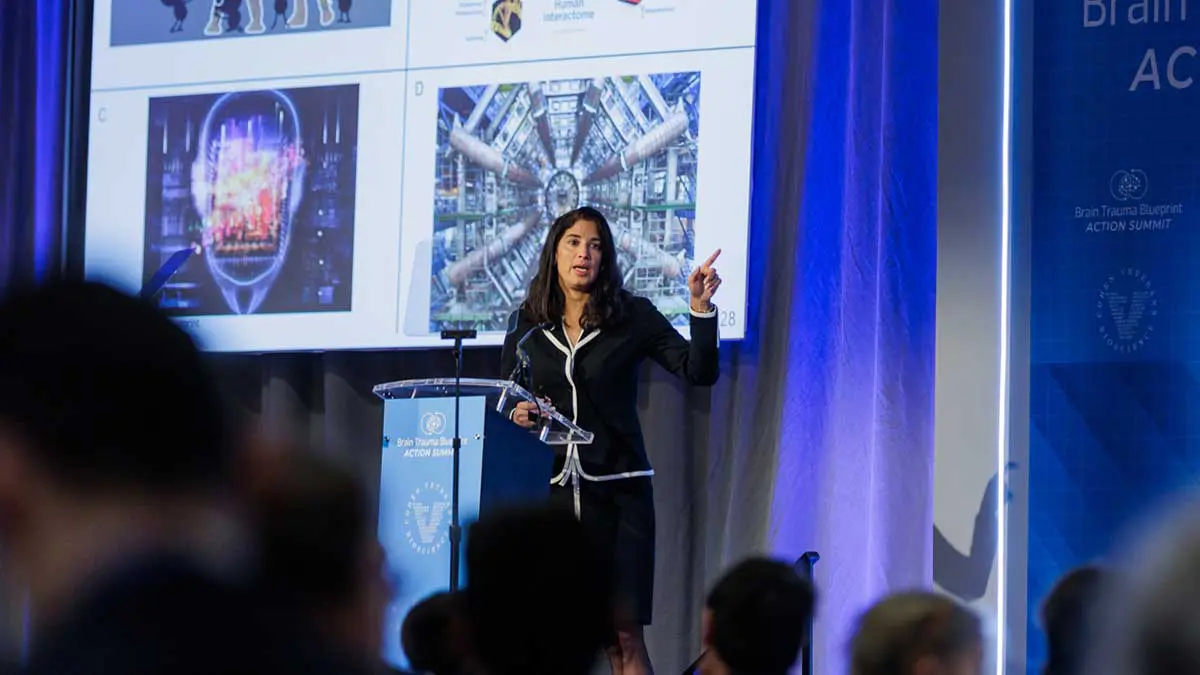
The Brain Trauma Blueprint is a framework that enables stakeholder groups across government, academia, foundations, and industry to advance precision diagnostics and treatments for brain trauma through a coordinated effort. The framework comprises a 12-step process to jointly identify unmet patient needs, associated research priorities, landscape state of the science, identify research gaps and barriers and provide recommendations for progress. The framework also provides a call to action for funders and collaborators across the broader stakeholder community to engage in a transparent & coordinated network.
Advancing TBI Care Through a Research Roadmap
Authored by leading experts in the traumatic brain injury (TBI) field, the six-part series is being published in the Journal of Neurotrauma and will lay the framework for a roadmap to advance the field, based on a State-of-the-Science consensus conference held in 2019 with >125 leaders in the field. The first installment focuses on the complex nature of brain trauma and how variability in clinical presentation (phenotypes) has confounded research. The consensus roadmap recommended that a streamlined method for characterizing data collected in different settings could lead to more targeted care and improved patient outcomes.
As a direct outcome of the collaboration fostered through the Blueprint, CVB and its collaborators have developed the first of a suite of tools to capture the variability of subject-level data across the spectrum of TBI. Using this standardized approach, the new tool, PhenoBench, is made freely available via a public code repository to enable researchers to evaluate phenotyping data collected across different studies.
“TBI presents differently from one patient to the next, and so it is important to have the ability to predict who might recover versus who is susceptible to long-term effects. This set of tools is anticipated to provide researchers with the means to standardize how they analyze and subsequently interpret TBI phenotyping data across different patient populations,” said Lee Lancashire, PhD, CVB Chief Information Officer, and collaborating author on the publication. “We expect PhenoBench to have a significant impact on the field by ensuring that new and existing data can be used to discover reproducible and transparent signatures of patient phenotypes. This will enable prediction of TBI outcomes and move us closer to tailored treatments that improve recovery.”
Toward a Personalized Approach to TBI Care
TBI is a leading cause of death and disability in the U.S. Yet despite the personal, economic, and societal costs of TBI, as well as the significant research investments to date, there are no FDA-approved treatments that address the long-term consequences many individuals who have sustained a TBI will go on to develop. Although most individuals who experience a TBI recover, a significant subset have persistent symptoms, including mental health conditions, sleep disturbances, and memory impairment, further increasing the personal and economic burden. Many researchers believe that studying the clinical features‚ or phenotype, of patients who recover from a TBI versus those who develop chronic effects could lead to better, more personalized treatment options for all TBI patients.
To understand the challenges of a phenotype-based strategy for TBI care, the authors of the Journal of Neurotrauma’s first Brain Trauma Blueprint publication‚ Phenotyping the Spectrum of Traumatic Brain Injury: A Review and Pathway to Standardization [10.1089/neu.2021.0059] describe the current research on approaches to patient phenotyping, and the need to consider new approaches such as unsupervised machine-learning, a type of artificial intelligence that looks for patterns and similarities across vast amounts of data without needing to know the clinical outcomes.
According to Mary Jo Pugh, PhD, RN, professor in the Department of Medicine, Division of Epidemiology at the University of Utah School of Medicine and Investigator at the Informatics, Decision-Enhancement and Analytic Science Center of Innovation at the VA Salt Lake City and lead author on the manuscript, “Phenotyping is becoming an increasingly popular approach to the evaluation of TBI and trajectories of TBI-related outcomes. It has great potential to identify the right patient for the right treatment at the right time.”
Additional authors on the publication include Eamonn Kennedy, PhD (Univ of Utah, developer of PhenoBench), Eric M Prager, PhD (Cohen Veterans Bioscience), Jeffrey Humpherys, PhD (Univ of Utah), Kristen Dams-O’Connor, PhD (Mount Sinai), Dallas Hack, MD (ret. Col. Army), Mary Katherine McCafferty (Univ of Utah) Jessica Wolfe, PhD, MPH (Cohen Veterans Bioscience), Kristine C. Yaffe, MD (UCSF), Michael McCrea, PhD (Medical College of Wisconsin), Adam R. Ferguson, PhD (UCSF), Lee Lancashire, PhD (Cohen Veterans Bioscience), Jamshid Ghajar, MD, PhD (Stanford), Angela Lumba-Brown, MD (Stanford).
Other publications in the series will cover key domains identified as barriers to progress: epidemiology, basic research, biomarker discovery and validation, clinical trial design, and clinical guideline implementation. Altogether, the TBI Precisions Solutions Roadmap will guide the development of actionable research priorities that frame the next phase of the roadmap over the coming months.
View this press release on PR Newswire